About the Program
Learn about the unique aspects of our program...
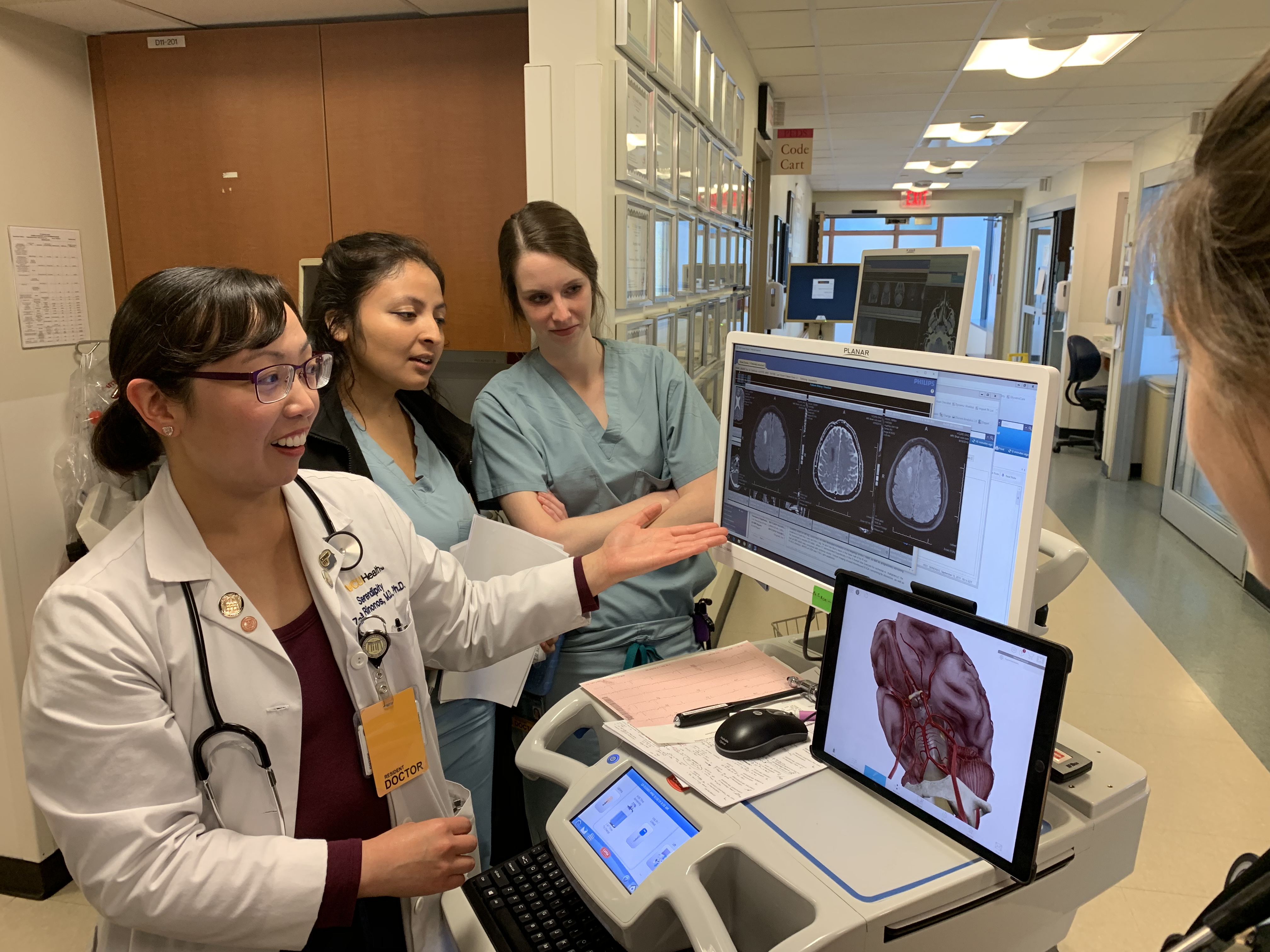
Welcome to the Department of Neurology at VCU School of Medicine’s residency program!
 We are delighted that you’re pursuing a career in neurology, a fascinating and dynamic field currently undergoing an incredible period of growth and discovery.
We are delighted that you’re pursuing a career in neurology, a fascinating and dynamic field currently undergoing an incredible period of growth and discovery.
Our residency program provides world-class clinical training in a supportive and collegial environment while ensuring our graduates obtain the skills they need to become leaders and pioneers in the field of neurology.
You can expect a comprehensive education in the diagnosis and management of common and rare neurological diseases in a diverse patient population. Skilled clinicians, researchers and educators who are deeply invested in your educational development and success will provide guidance and mentorship throughout your time at VCU.
Our program is designed with flexibility, and we encourage you to pursue educational opportunities and personal growth outside of your core clinical training. This gives you the chance to explore interests you may have in areas such as subspecialty care, research, education and international medicine.
 Just as this is an exciting time to be a neurologist, it’s an especially exciting time to be at VCU. Our department is experiencing a period of growth and development, allowing even more opportunities for our residents as they pursue careers in neurology. We're actively expanding our already robust complement of subspecialists and the residency program has grown to include eight residents. We're excited for you to contribute your own passions, interests and talents to the growing department and leave your mark on the residency program.
Just as this is an exciting time to be a neurologist, it’s an especially exciting time to be at VCU. Our department is experiencing a period of growth and development, allowing even more opportunities for our residents as they pursue careers in neurology. We're actively expanding our already robust complement of subspecialists and the residency program has grown to include eight residents. We're excited for you to contribute your own passions, interests and talents to the growing department and leave your mark on the residency program.
Warmly,
Education Leadership
Leadership
Faculty Leadership...

Stephanie Bissonnette, D.O., MPH
Associate Vice-Chair of DEI, Assistant Professor

Stephanie Bissonnette, D.O., MPH
Associate Vice-Chair of DEI, Assistant Professor
Department of Neurology
Movement Disorders
Phone: (804) 828-7929

Taylor Haight, M.D.
Assistant Professor Associate Program Director, Education

Taylor Haight, M.D.
Assistant Professor Associate Program Director, Education
Department of Neurology
Division of Vascular and Critical Care Neurology
Phone: (804) 828-7929
Email: Taylor.Haight@vcuhealth.org
Learn more about VCU's Department of Neurology Residency Program
Rotations
The Department of Neurology operates on a 13-block rotation schedule...
Each of the 13 blocks consists of 2 separate 2-week rotations
PGY1: All residents who match into our program also receive a preliminary intern year in internal medicine at VCU. We have worked closely with our IM colleagues to craft an intern year that gives a strong foundation in medicine with rotations of particular relevance to future neurologists (including palliative care, hematology/oncology, and Neuroscience ICU experiences), as well as begins to prepare our preliminary residents for their neurology years. Preliminary residents rotate through the Neuroscience ICU and Stroke consult team, and also have a 2 week “neurology boot camp” block at the end of their intern year. Please see click here for more details on the preliminary year and a sample schedule.
PGY2: The goal of our PGY-2 year is to acclimate our residents to the care of acute neurologic conditions in the inpatient setting, while also giving them ample outpatient and elective experiences early in their training. This combination allows our residents to start their training with a well-rounded knowledge of neurology, while helping allowing them to begin exploring their specific interests. Roughly half their year is spent on inpatient services (Wards, Consults, Day float, Night float, and at the Veterans Affairs Medical Center consult team. The other half is spent on electives and outpatient rotations (including EMG, EEG, movement disorders, and neuro-ophthalmology).
PGY-3 and PGY-4: Our residents continue to develop graduated leadership responsibilities during these years, with PGY-3 residents taking on senior roles by the second half of the year. Residents continue to have ample elective and outpatient time in addition to their roles as inpatient team leaders, and also incorporate time in child neurology, psychiatry, and Neuroscience ICU.
Please click here for the Residency Yearly Schedule sample.
Residents rotate through the following:
Neurology Inpatient Services
Two inpatient neurology teams, one a General Neurology Service (seizures/status epilepticus, Multiple Sclerosis, AIDP, CNS cancers, Myasthenia Gravis, autoimmune encephalitis, etc) and one a Stroke Service. Each team consists of a neurology faculty member, senior resident, junior resident, psych intern, and a nurse practitioner. Residents lead the care of the patient, overseen by the attending faculty member. Members of the neurology inpatient teams work with the Neuroscience Intensive Care Unit (NSICU) team to co-manage critically ill neurological patients, and residents on the inpatient teams are also part of the pool of doctors responding to and managing acute stroke alerts, as well.
Neurology Consultation Services
The consult team, consisting of a neurology faculty member, senior resident, junior resident, nurse practitioner, and sometimes other rotating residents (medicine, neurosurgery, PM&R, etc). The team handles consults from other inpatient services and the Department of Emergency Medicine, with residents on the consult service also being in the pool to respond to acute stroke alerts. This is one of the most active consultation services at the hospital, with a wide breadth and depth of neurological conditions.
Neuroscience Intensive Care Unit (NSICU)
Residents rotate through the NSICU during PGY-1, PGY-3, and PGY-4 under the supervision of NSICU intensivist faculty. On this rotation, residents learn to diagnose and manage critically ill patients with acute neurological conditions, including strokes, status epilepticus, myasthenic crisis, and encephalitis; patients are co-managed with the neurology inpatient team. Residents have hands-on opportunities to perform and become certified in a number of procedures, such as line placements.
Epilepsy and Electroencephalogram (EEG)
Residents learn to perform and interpret routine and long-term EEG monitoring, for both adult and pediatric patients. In addition to reading EEGs, residents will also see epilepsy patients in clinic and receive instruction on the medical and surgical management of epilepsy syndromes. Neurology residents complete a minimum of two months of EEG training during their time in the program.
Neuromuscular and Electromyography (EMG)
During a minimum of two months of EMG training, residents receive hands-on education in the diagnosis of neuromuscular conditions and their management. Residents gradually obtain more responsibility in performing nerve conduction studies and EMG, and after four weeks of training, they will be able to independently perform their own EMG procedures while under supervision.
In addition to performing EMGs, residents will also see patients in neuromuscular clinics, including the multidisciplinary amyotrophic lateral sclerosis (ALS) clinic.
Central Virginia VA Healthcare System
The neurology services available at the Richmond-area Veterans Affairs hospital are integral to the Department of Neurology and its residency program. The rotations involve managing the inpatient service, consultations and EEG interpretation, plus they engage in neurology outpatient general and subspecialty clinics.
Day Float
The Day float resident is a PGY-2 who works with the consult team from 12PM-8PM Monday through Thursday, and 7AM-5PM on Saturday and Sunday; the Day Float has Friday off. This resident sees new consults in conjunction with the consult team, is in the pool for responding to acute stroke alerts, and also assists the inpatient team with procedures (LPs, etc) and education of residents and medical students.
Night Float
The night float rotation is two weeks long, consisting of in-house overnight call from Sunday to Friday nights from 8PM-9AM, with Saturday night off. One junior and one senior neurology resident are on night float together and they see emergency consults (including acute stroke alerts), as well as cover the inpatient neurology services.
All consults are staffed via phone overnight with a neurology faculty member. Night float residents present any admissions to the day team in the morning and go home by 9 a.m.
Outpatient Neurology
Our program is unique in that as part of our core curriculum, we provide residents with ample time in several dedicated outpatient subspecialty rotations, starting early in their training and continuing throughout their residency.
Part of this outpatient experience consists of an Ambulatory Care Center rotation, where residents can explore a variety of outpatient neurology subspecialty clinics of their choosing over the course of the two-week block.
Throughout their three years of training, residents also maintain a half-day per week of their own continuity clinic.
Pediatric Neurology
Residents manage inpatient and emergency room consults and advise the inpatient pediatric team. During this rotation, residents gain broad experience in the management and treatment of pediatric neurological disorders including epilepsy, developmental abnormalities and metabolic disorders. They are directly overseen by faculty specializing in pediatric neurology.
Psychiatry
PGY-4 residents will spend 4 weeks as members of the psychiatry consult-liaison services at VCU Medical Center. This rotation exposes residents to the diagnosis and management of acute and chronic psychiatric conditions including delirium, depression, anxiety, psychosis, personality disorders and suicidality, plus the intersection of psychiatric conditions and a variety of medical conditions.
Scholarly Activity
All residents will participate in scholarly activity during their residency. All PGY-3’s present a case at the yearly Night of the Cases dinner (with the highest rated resident receiving a free trip to present their case at the annual Virginia Neurological Society meeting at the Omni Homestead resort). All PGY-4’s present at the departmental Grand Rounds. In addition, residents are encouraged to participate in a research project during their residency, under the guidance of a faculty research mentor of their choosing. Previous research projects have included basic and translational research, clinical research, outcomes and health utilization, education, health care disparities and clinical case presentations with literature review. Residents will also receive training from their research mentors in topics of study design, funding and implementation.
Electives
In addition to the required outpatient rotations detailed above, additional elective time is provided during the 3 years of residency. Potential electives include (but are not limited to):
- Neuro-radiology
- Neuro-Ophthalmology
- Neuro-pathology
- Neurosurgery
- Headache/chemo-denervation
- Movement disorders
- Epilepsy
- Neuro-cognitive/Dementia
- Sleep
- Neuromuscular
- Neuro-Oncology
- Global Health Neurology
- Tele-neurology
- TBI
- Pain Medicine
- Speech and Language Pathology
Residents may also use elective time to become more adept at electrodiagnostic tests like EMG, EEG, or to further pursue scholarly projects.
Didactics
Learning opportunities...
Throughout the three-year program, residents take part in a multitude of didactic lectures and conferences facilitated by a combination of residents and faculty with expertise in the topics at hand.
Current and upcoming didactic opportunities include:
- Journal club
- Morning report
- Comprehensive subspecialty series exploring the neuroanatomy, neuropathology, clinical presentations and management of a variety of neurological conditions
- Grand rounds
- Subspecialty conferences in neurovascular, neuromuscular, epilepsy, movement disorders, and quality improvement.
- Updates in the field of neurology
- The business of neurology
- The ethics of neurology
- Joint Neurology/Neurosurgery Case Conference
- Neuroimaging Conference
- Localization Rounds
FAQs
Frequently asked questions about our program...
Yes! We work with each resident early in their training to connect each resident to a faculty mentor that is a good fit for their particular interests and career goals; mentors meet with our residents at least quarterly to discuss topics such as progress, career interests, and research. In addition to this, we connect our residents into less formal mentoring groups we call "Neuro Families", consisting of a resident from each year plus a faculty mentor; these groups do fun activities outside of work at least quarterly, and allow residents at different stages of their training to mentor one another.
The majority of our residents pursue fellowship, and we have had a 100% success rate in the past few years for our residents getting into their desired subspecialty, either at VCU or nationally. Recently graduating residents have been accepted to fellowships in neurovascular, epilepsy, neuro-oncology, sports neurology, movement disorders, neuro-physiology, and neuromuscular (to name a few).
The VCUHS GME Website (for residents & fellows) has detailed information about current housestaff salary, contract and benefits. The website also provides links to view information on various policies and overall information about VCUHS and the city of Richmond. For more information, please click on the link to see 2020 Benefits.
Every resident gets 3 weeks of vacation per year, as well as additional time off around either Christmas or New Year’s.
Yes, we offer visiting electives for 4th year medical students from other medical schools, organized through the VCU School of Medicine Dean's Office.
Yes, our residents have been involved in activities such as Neurology on the Hill (visiting congressmen in DC, etc), and other health advocacy initiatives.
One of the most important questions you can ask! In additional to the variety of options at the hospital cafeteria itself, the hospital has a full service Chick-Fil-A, Subway, and a 24/7 Panera Bread. There are also a variety of food carts available directly outside the main hospital on weekdays.
Residents have access to the covered parking deck (D Deck) directly connected to the health system.
Contact
Neurology Residency Program
Residency Application Questions
Yes. While technically we are an Advanced program in the Match, if you match with VCU neurology, then you automatically receive a preliminary year internship with the VCU department of Internal Medicine as well. You do NOT need to apply for an interview with the Internal Medicine department separately, but you DO need to rank them as your intern year for the final Match. When ranking the Neurology Prelim position use NRMP code 1743140P1.
We sponsor J-1 visas only.
- Applicants must be within 4 years of graduating medical school, or be within 4 years of direct patient care activities (independent practitioner or trainee); observerships or research do not count. Applicants must also have at least 3 months of direct patient care in the US within the last 4 years.
- Applicants must have at least 3 letters of recommendation from US or Canadian physicians that can speak to the applicant’s clinical skills and personal characteristics. A chair letter is not required, and all of the letters don’t need to be from neurologists (though we suggest that least one of them be).
Our Neurology program participates in the NRMP Main Residency Match, www.nrmp.org(link is external) and in the Electronic Residency Application Service (ERAS) www.aamc.org/eras(link is external). Applicants must register with both NRMP and ERAS to participate in the services of each.
For the 2020-2021 interview season, all interviews will be done virtually.
Interview season runs from late October 2021 to mid January 2022. Interviews are half-days, in addition to an optional virtual meet and greet with residents on the night before the interview. If you are unable to attend the meet & greet the night before we offer an additional meet & greet the day of your interview.
Message from the Chiefs
Welcome to VCU Neurology Residency Program...
-500x375.jpg)
Welcome to the VCU Neurology Residency Program!
As a prospective resident, we feel that there are a few things that should be highlighted about our wonderful program. First and foremost, you would be joining an amazing group of residents, attendings, and advanced practice providers whose primary focus is the continued growth and education of our residents. We foster an environment of camaraderie both on the wards and outside of work. As a large tertiary care center, our catchment radius ensures that we are exposed to a wide array of both common and extremely rare neurological diseases, fostering a perfect environment for continued hands-on learning.
The Department of Neurology at VCU is continually expanding, with nearly every subspecialty of neurology represented, offering a comprehensive outpatient neurology experience that gives our residents a chance to determine their career goals early in the course of their residency. The combination of amazing colleagues, wide breadth of pathology, and first-class clinical experiences is what makes VCU such an amazing place to train.
We thank you for considering our program, and we hope to see you soon. If you have any questions about our program or Richmond in general, please feel free to contact us!
Sincerely,
Residents
Meet our current residents...
VCU Health System, Department of Neurology Housestaff are listed below
PGY-1
.jpg)
Peter Felton, MD
PGY-1
.jpg)
Peter Felton, MD
PGY-1
Department of Neurology
Medical School Attended: Case Western Reserve School of Medicine

Nashira Howe, MD
PGY-1

Nashira Howe, MD
PGY-1
Department of Neurology
Medical School Attended: Tulane University School of Medicine
.jpg)
Hasti Izadpanah, DO
PGY-1
.jpg)
Hasti Izadpanah, DO
PGY-1
Department of Neurology
Medical School Attended: Edward Via College of Osteopathic Medicine
Lucy Jin, MD
PGY-1
Lucy Jin, MD
PGY-1
Department of Neurology
Medical School Attended: Virginia Commonwealth University School of Medicine
.jpg)
Cheryne Kim, MD
PGY-1
.jpg)
Cheryne Kim, MD
PGY-1
Department of Neurology
Medical School Attended: Oakland University William Beaumont School of Medicine
.jpg)
Emma Parolisi, MD
PGY-1
.jpg)
Emma Parolisi, MD
PGY-1
Department of Neurology
Medical School Attended: Virginia Commonwealth University School of Medicine

Brian Pok, MD
PGY-1

Brian Pok, MD
PGY-1
Department of Neurology
Medical School Attended: Virginia Commonwealth University School of Medicine
.jpg)
Hitesh Vaishnav, DO
PGY-1
.jpg)
Hitesh Vaishnav, DO
PGY-1
Department of Neurology
Medical School Attended: Lincoln Memorial University, DeBusk College of Osteopathic Medicine

Lauren Gebhardt, DO
PGY-1 Child Neurology

Lauren Gebhardt, DO
PGY-1 Child Neurology
Department of Neurology
Medical School Attended: Liberty University College of Osteopathic Medicine
PGY-2

Brianne Kelly, DO
PGY-2

Brianne Kelly, DO
PGY-2
Department of Neurology
Medical School Attended: Lincoln Memorial University - DeBusk College of Osteopathic Medicine

Diana Marzouk, DO
PGY-2

Diana Marzouk, DO
PGY-2
Department of Neurology
Medical School Attended: West Virginia School of Osteopathic Medicine

Monica Prudencio, MD
PGY-2

Monica Prudencio, MD
PGY-2
Department of Neurology
Medical School Attended: University of Virginia School of Medicine

Nicholas Edwards, MD
PGY-2

Nicholas Edwards, MD
PGY-2
Department of Neurology
Medical School Attended: Creighton University School of Medicine

Jasmine Hinaman, MD
PGY-2

Jasmine Hinaman, MD
PGY-2
Department of Neurology
Medical School Attended: Oakland University William Beaumont School of Medicine

Akila Khan, MD
PGY-2

Akila Khan, MD
PGY-2
Department of Neurology
Medical School Attended: University of Illinois College of Medicine - Rockford

Alejandro Jimenez Quintero, MD
PGY-2

Alejandro Jimenez Quintero, MD
PGY-2
Department of Neurology
Medical School Attended: Universidad Central del Caribe School of Medicine

Skylar Jones, DO
PGY-2

Skylar Jones, DO
PGY-2
Department of Neurology
Medical School Attended: Edward Via College of Osteopathic Medicine - Carolinas Campus

Prateek Sharma, DO
PGY-2 Child Neurology

Prateek Sharma, DO
PGY-2 Child Neurology
Department of Neurology
Child Neurology
PGY-3
.jpg)
JoBeth Bingham, DO
PGY-3
.jpg)
JoBeth Bingham, DO
PGY-3
Department of Neurology
.JPG)
Brendan Parr, DO
PGY-3
.JPG)
Brendan Parr, DO
PGY-3
Department of Neurology

Manisha Kotay, MD
PGY-3

Manisha Kotay, MD
PGY-3
Department of Neurology

Noor Mozahem, MD
PGY-3

Noor Mozahem, MD
PGY-3
Department of Neurology

Saba Nawaz, MD
PGY-3

Saba Nawaz, MD
PGY-3
Department of Neurology

Kelly Nicol, DO
PGY-3

Kelly Nicol, DO
PGY-3
Department of Neurology

Jillian Prier, MD
PGY-3

Jillian Prier, MD
PGY-3
Department of Neurology

Cole Weinstein, DO
PGY-3

Cole Weinstein, DO
PGY-3
Department of Neurology

Miranda Creasey, MD
PGY-3 Child Neurology

Miranda Creasey, MD
PGY-3 Child Neurology
Child Neurology
PGY-4

Mckenzye Dehart-McCoyle, DO, PGY-4
Chief Resident

Mckenzye Dehart-McCoyle, DO, PGY-4
Chief Resident
Department of Neurology
Medical School Attended: Edward Via College of Osteopathic Medicine

Ryan Naum, DO, PGY-4
Chief Resident

Ryan Naum, DO, PGY-4
Chief Resident
Department of Neurology
Medical School Attended: West Virginia School of Osteopathic Medicine

Michael Todd, MD, PGY-4
Chief Resident

Michael Todd, MD, PGY-4
Chief Resident
Department of Neurology
Medical School Attended: Edward Via College of Osteopathic Medicine

Ryan Lamb, DO
PGY-4

Ryan Lamb, DO
PGY-4
Department of Neurology
Medical School Attended: Lake Erie College of Osteopathic Medicine

Haripreet Mayo, MD
PGY-4

Haripreet Mayo, MD
PGY-4
Department of Neurology
Tri Nguyen, MD
PGY-4
Tri Nguyen, MD
PGY-4
Department of Neurology
Medical School: Western University of Health Sciences College of Osteopathic Medicine of the Pacific

Shital Patel, MD
PGY-4

Shital Patel, MD
PGY-4
Department of Neurology
Medical School Attended: Geisinger Commonwealth School of Medicine
Victoria Phoumthipphavong, MD
PGY-4
Victoria Phoumthipphavong, MD
PGY-4
Department of Neurology
Medical School Attended: USF Health Morsani College of Medicine

Mehreen Shahid, MD
PGY-4, Child Neurology

Mehreen Shahid, MD
PGY-4, Child Neurology
Department of Neurology
Medical School Attended: Edward Via College of Osteopathic Medicine
PGY-5
Darina Dinov, DO
PGY-5 Child Neurology
Darina Dinov, DO
PGY-5 Child Neurology
Department of Neurology
Child Neurology
Jane Chang, MD
Clinical Neurophysiology Fellow
Jane Chang, MD
Clinical Neurophysiology Fellow
Neurology
Medical School Attended: Medical College of Georgia
Residency: Virginia Commonwealth University

Diana Hancock, MD
Movement Disorders Fellow

Diana Hancock, MD
Movement Disorders Fellow
Neurology
Medical School Attended: Brody School of Medicine at East Carolina University
Residency: Northwell Health North Shore/Long Island Jewish Hospitals
An Cao, MD
Neuroimmunology Fellow
An Cao, MD
Neuroimmunology Fellow
Neurology
Medical School Attended: University of Kansas School of Medicine
Residency: Wright State University Boonshoft School of Medicine

Isabel Narvaez Correa, MD
Neuromuscular Medicine Fellow

Isabel Narvaez Correa, MD
Neuromuscular Medicine Fellow
Neurology
Medical School Attended: University of Cuenca, Ecuador
Residency: Texas Tech University Health Sciences Center

Peter Pacut, MD
Neuromuscular Medicine Fellow

Peter Pacut, MD
Neuromuscular Medicine Fellow
Neurology
Medical School Attended: Jagiellonian University Medical College
Residency: Chief Resident, University of Massachusetts

Brooke Kubat, MD
Vascular Neurology Fellow

Brooke Kubat, MD
Vascular Neurology Fellow
Neurology
Medical School Attended: University of North Dakota
Residency: University of Iowa




